Dental Insurance
Cigna Dental Care® Health Maintenance Organization (HMO) Prepaid Plan
 800.997.1617
800.997.1617
24/7
Cigna.com/stateoftn
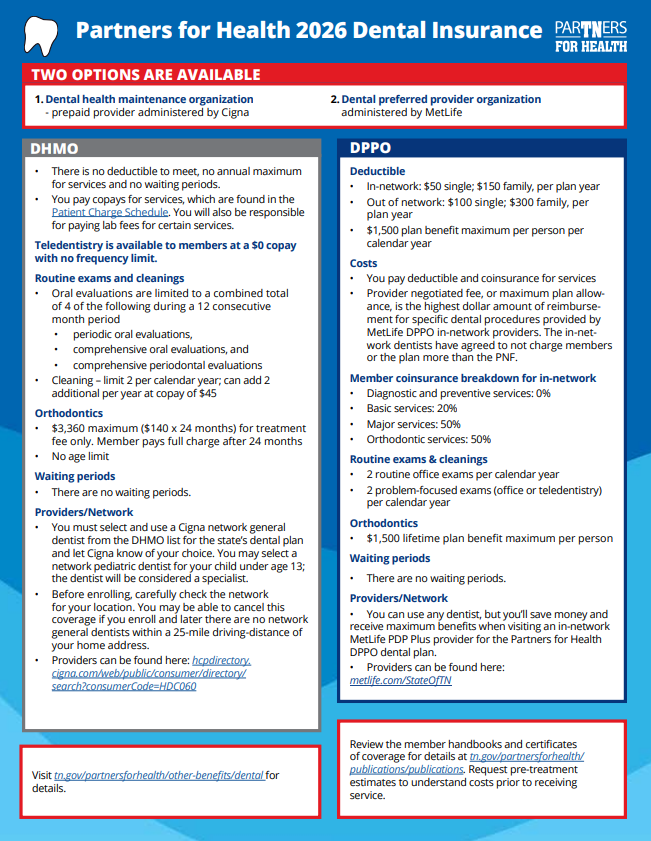
- You must select and use a Cigna network general dentist from the DHMO list for the state’s dental plan and let Cigna know of your choice.
- You must use your selected dentist to receive benefits.
- You may select a network pediatric dentist as the network general dentist for your dependent child under age 13. The pediatric dentist will be considered a “specialist” for plan benefits. At age 13, you must switch the child to a network general dentist or pay the full charge from the pediatric dentist.
- There may be some areas in the state where network general dentists are limited or not available. Before enrolling, carefully check the network for your location.
- With the DHMO, you may be able to cancel this coverage if you enroll and later there are no network general dentists within a 25-mile radius of your home address.
- You pay copays for dental treatments. Review the Patient Charge Schedule under Publications and Dental HMO - Prepaid Provider at https://www.tn.gov/partnersforhealth/publications/publications.html before having procedures performed.
- Lab fees may apply for some procedures and are the responsibility of the member to pay.
- No deductibles to meet, no claims to file, no waiting periods, no annual dollar maximum.
- Preexisting conditions are covered.
- Referrals to specialists by network general dentists are required.
- Teledentistry is offered at no charge.
- For orthodontic services in progress, members should contact Cigna customer service for additional information regarding their benefit.
- See the Certificate of Coverage (PDF) under Publications and Dental HMO - Prepaid Provider at https://www.tn.gov/partnersforhealth/publications/publications.html for complete details.
- To learn about all DHMO benefits, find the Cigna DHMO handbook by clicking on Publications and Dental HMO – Prepaid Provider.
- Search for a provider
 855-700-8001
855-700-8001
7 a.m. to 5 p.m. CT
Metlife.com/StateOfTN
- You can use any dentist, but you’ll save money and receive maximum benefits when visiting an in-network DPPO provider for the state's dental plan.
- There are no waiting periods for any services.
- In-network deductibles will be $50 per individual and $150 per family with the DPPO.
- Two routine office exams and two problem-focused exams will be covered each calendar year.
- The orthodontia plan benefit lifetime maximum will increase to $1,500.
- See the Certificate of Coverage (PDF) for coverage details.
- To learn about all DPPO benefits, find the MetLife Dental DPPO handbook under Publications and Dental PPO.
- Search for a provider or find if your current provider is in Network - MetLife Dental DPPO:
- Access Metlife.com/stateoftn - you will first, select "Dental Insurance" scroll down and then, click “Find a Dentist.” Then, select "PDP Plus" from the dropdown labeled "Your Network" and key in a desired zip code and select find.
- You can choose to filter your results by Distance, Specialty, if they are accepting new patients, languages spoken, and more!